Cannabis and pathologies in dogs and cats: first survey of phytocannabinoid use in veterinary medicine in Argentina | Journal of Cannabis Research
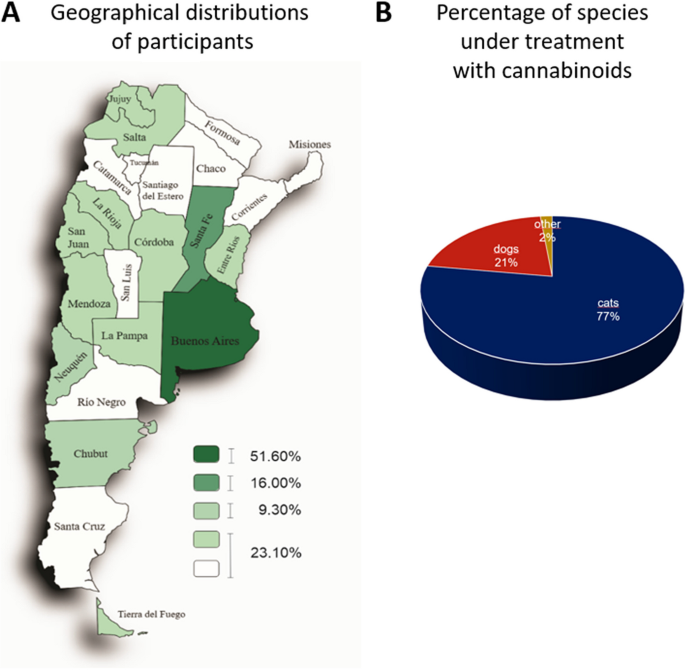
Analysis of the distribution of professionals in medicine veterinary along the country indicated that the highest percentage of veterinarians was concentrated in the provinces of Buenos Aires (51.60%) and Santa Fe (16%), followed by the Autonomous City of Buenos Aires (CABA) (9.30%) and the rest of the provinces (23.10%) (Fig. 1A). Sixty-seven percent of all professionals consulted mentioned that they were small animal generalists, including dogs and cats. Instead, 33% had different specialties such as nutrition, behavioral, ozone therapy, neural therapy, phytotherapy, surgery, nephrology, cat medicine, neurology, physiotherapy, anesthesiology, acupuncture, emergency medicine, and cardiology.
Participants of this survey and treated species. A Geographical distribution of veterinarians who participated. The density map shows the geographical distribution of professionals who conduct treatments using cannabinoids. Buenos Aires (51.60%) and Santa Fe (16.00%) concentrate the most significant number of professionals. CABA and Chubut account for 9.30% and the rest of the country 23.10%. Percentage of species under treatment with cannabinoids. B The pie chart shows that dogs compound 77% (n = 89), cats 21% (n = 24), and other species 2% (n = 2) of the total of 115 answers
Figure 1B shows that 77% of treated species corresponded to dogs (n = 89), 21% to cats (n = 24), and 2% to other species (one horse and one turtle). Following, we focused on dogs and cats. In the group of dogs, the most frequent breeds were German Shepherd, Labrador, Dachshund, French Bulldog, Beagle, Cocker, and mixed breeds. In the group of cats, the European Shorthair cat and the Persian and Siamese breeds were the most treated. Both dogs and cats were grouped according to age and the conditions they had. Diseases/conditions were identified through a precise diagnosis based on correct anamnesis and additional tests such as x-rays, laboratory tests, magnetic resonance imaging, and cytology.
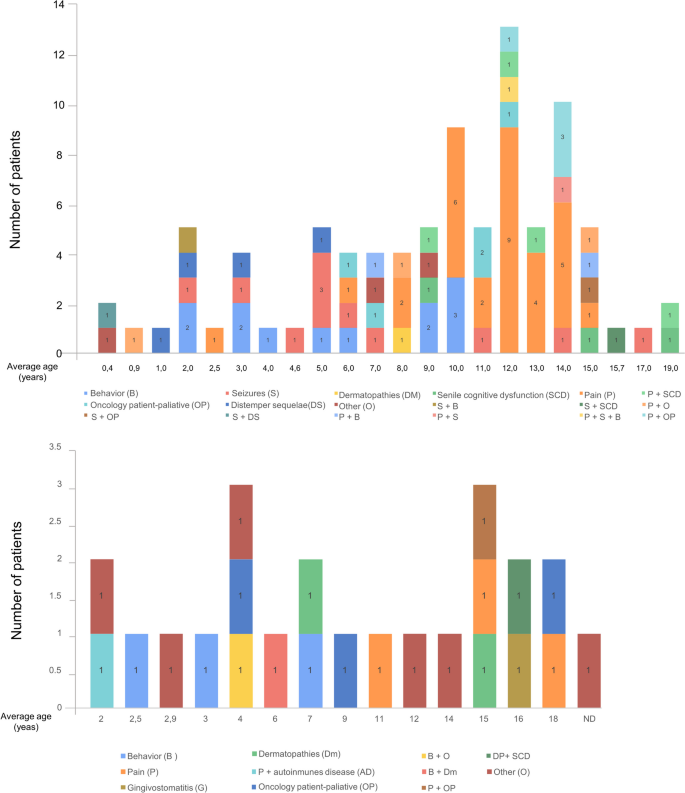
The upper graph in Fig. 2 shows that a higher proportion of dogs (n = 47) corresponded to animals between 9 and 14 years old. In this group, pain was the most prevalent symptom treated with phytocannabinoids (31 cases). Following that, behavioral disorders (12 cases) and seizures (n = 11) were the most frequent conditions. The remaining disorders/diseases included sequelae of distemper, cancer, senile cognitive dysfunction, dermatopathies, and combinations of two or more conditions. The term “other” included not listed pathologies/conditions in the structured question like obesity, arthrosis, tracheal collapse, intrahepatic shunt and metabolic disorder, and nervous and articular signs of leishmania infection.
Pathologies identified in dogs and cats. The graphic represents the distribution of the patients according to their age expressed in years. For each age, bars exhibit the number of patients with one or a combination of pathologies/conditions. P, pain; B, behavior; S, seizures; OP, oncology patient; DS, distemper sequelae; DM, dermatopathies; SCD, senile cognitive dysfunction; AD, autoimmune disease; G, gingivostomatitis; ND, non-determined age
Cats received in consultation (24 animals) were distributed over a wide age range similar to dogs (2–18 vs. 0.4–19 years, respectively) (Fig. 2, bottom graph). The diseases and conditions observed included behavioral disorders, pain, gingivostomatitis, dermatopathies, autoimmune diseases, and combinations of two or more conditions. Patients with asthma, idiopathic cystitis, and feline immunodeficiency virus were included in the term “other.” Since the number of patients was lower than in the dog group, there were no differences in the number of cases according to the disease/condition treated. However, pain, behavioral disorders, and cancer had three cases each.
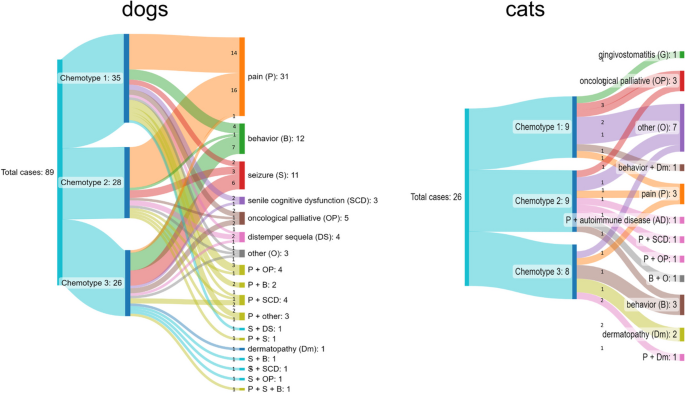
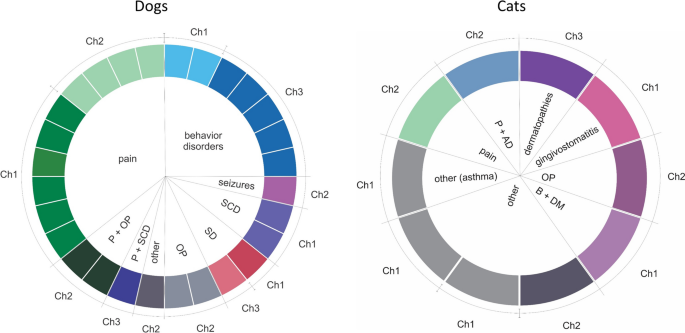
Full-spectrum cannabis extract derived from three different chemotypes was utilized. Chemotype 1 contained a higher THC concentration than CBD ([THC] > [CBD]), chemotype 2 was characterized by a similar concentration of both cannabinoids ([THC] = [CBD]), and chemotype 3 presented more CBD than THC ([THC] < [CBD]). Figure 3 shows chemotypes used to treat the different diseases for dogs (left) and cats (right). The route of administration was oral transmucosal.
In dogs, 97% of patients with pain were treated with chemotypes 1 and 2 (45%, n = 14 and 52%, n = 16, respectively), while chemotype 3 was less used (3% of patients, n = 1). Doses were adjusted throughout treatment in order to observe improvement in clinical signs. The dose range was between 1 and 18 drops/day for chemotype 1, with average values between 6 and 7 drops from the beginning of treatment to 60 days. For chemotype 2, the dose range was between 1 and 12 drops/day, with mean values between 3 and 6 drops. On the other hand, 58% of dogs (n = 7) with behavioral disorders received chemotype 3. Chemotype 1 was used in 33% (n = 4) and chemotype 2 in 8% of patients (n = 1) with this condition. Chemotype 3 was also utilized in 54% of patients with seizures (n = 6). The dose range of chemotype 3 was between 2 and 10 drops/day with mean values of 4 to 6 drops. In cats, chemotypes 1 and 2 were used for various conditions. Behavioral disorders (n = 2) and dermatopathies (n = 2) were preferentially treated with chemotype 3. The dose range for all chemotypes was between one and four drops/day with mean values of two drops.
Among the dogs, a subgroup received previously analyzed oil, and the concentrations of the most relevant cannabinoids were determined by chromatography. Table 1 summarizes the initial daily dose of THC and CBD received by patients treated with these oils, adjusted according to the weight of each individual. The conditions with the highest prevalence and the most commonly used chemotype are shown. For example, of the 31 patients with pain, 14 had been treated with chemotype 1, and 10 received one analyzed oil. The mean dose/kg/day for this group of patients was THC: 0.083 ± 0.037 and CBD: 0.025 ± 0.018. In addition, the table indicates the doses of chemotype 2 used for pain and chemotype 3 for behavioral disorders and seizures. The dosage was adjusted by increasing or decreasing the number of drops/day throughout the treatment.
Response to the treatment was only based on the clinical signs observed in consultation by the veterinarian and the information reported by the owner as symptoms. Column 2 of Table 2 shows signs and complementary diagnostic tests utilized for diagnosis, while columns 3 and 4 summarize signs/symptoms evaluated during the treatment.
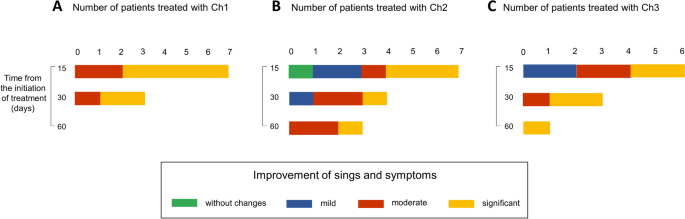
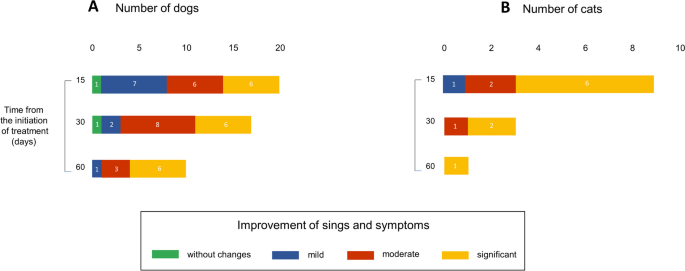
We collected information on patients who were in treatment for 15, 30, or 60 days at the time of the survey and classified the perception of the clinical status of patients according to indicators established by the professionals in the consultations. Improvements were classified into the following categories: no change, mild, moderate, and significant.
Among dogs treated for pain with chemotype 1, 36% (n = 4) showed mild, 27% (n = 3) moderate, and 37% (n = 4) significant improvement at 15 days of treatment. At 30 days, 50% (n = 4) showed moderate, and at 60 days, 80% (n = 4) exhibited significant improvement (Fig. 4A). In the group that received chemotype 2, 75% (n = 9) of patients showed significant improvement after 15 days of treatment (Fig. 4B). Those treated for seizures and behavioral disorders with chemotype 3 showed mild, moderate, and significant improvement (Fig. 4C and D). All data correspond to the number of patients evaluated at the moment of the survey. For this reason, the results did not include the complete monitoring of all patients.
Improvement in dogs along the treatment. The use of cannabinoids alone or combined with other medications improved clinical parameters. A scale was created to classify the improvement in middle, moderate, significant, or without changes. Bars represent the number of patients for each category. More prevalent diseases/conditions and the chemotype (Ch) used are shown. A Pain and Ch1. B Pain and Ch2. C Seizure and CH3. D Behavior disorders and Ch3. Patients were evaluated at 15, 30, and 60 days of treatment at the moment of the survey
For the group of cats, the initial daily doses of THC and CBD for those oils that were analyzed are summarized in Table 1. Chemotypes 1 and 2 were applied for pathologies such as behavioral disorders, pain, and cancer and within the category “other”: gingivostomatitis and asthma. Chemotype 3, in addition to the above, included dermic pathologies.
We evaluated the improvement according to the chemotypes used. For chemotype 1, 66% (n = 4) showed marked improvement at 15 days (Fig. 5A). For chemotype 2, patients with mild, moderate, and marked improvement were observed, as well as one case with no change (Fig. 5B). For chemotype 3, the percentage of patients with significant improvement was 43% (n = 3) at 15 days and 75% (n = 3) at 30 days (Fig. 5C). Like in dogs, all data about the cat group correspond to the number of patients evaluated at the moment of the survey.
Improvement in cats along the treatment. The use of cannabinoids alone or combined with other medications improved clinical parameters. We classify the improvement in middle, moderate, significant, or without changes. Bars represent the number of patients for each category. Due to that, the number of patients was reduced compared to the dog group, and there is no prevalent pathology. Data were classified according to the chemotype used. A, Ch1, B Ch2, and C CH3. Patients were evaluated at 15, 30, and 60 days of treatment at the moment of the survey
In the dog group, 28 out of 89 animals received cannabis oil extract as monotherapy. For pain treatment, cannabis as monotherapy was delivered to 10 of the 31 patients with this condition. Eight out of 11 animals received the extract for behavior disorders, and other individual cases were treated only with cannabis oil. For behavior disorders, six of seven animals were given cannabinoids as a single therapy. Figure 6A summarizes data showing which chemotype was used in each case. We compared doses of cannabinoids in polymedicated patients with doses applied to the other group that received it as single therapy. Supplemental Tables 1 and 2 show values for all chemotypes utilized for the most relevant conditions. Doses of cannabinoids were received for polymedicated patients, and the group that received only cannabinoid preparations was not significantly different. In all cases, veterinarians and caregivers reported a positive perception of treatments indicating moderate and significant improvement in the quality of life at 15, 30, and 60 days (Fig. 7A).
Dogs and cats treated only with cannabinoids. Pie graphs show the number of patients with one or a combination of pathologies and the chemotype used. P, pain; OP, oncologic patient palliative; DS, distemper sequela; SCD, senile cognitive dysfunction; B, behavior disorders; DM, dermatopathy; and AD, autoimmune disease
In order to evaluate whether chemotype 1 or chemotype 2 was the most appropriate for the treatment of pain, we compared the number of animals that showed significant improvement to those that showed mild/moderate improvement after 15 days treated with chemotypes 1 or 2. The relationship between these variables was not significant, Χ2 (1, N = 23) = 3.4862, p = 0.061. Therefore, both chemotypes relieved the symptoms.
The adverse effects reported in dogs were sedation and a case of a paranoid state in a poly-medicated patient with a behavioral disorder. The veterinarian replaced the oil with another one of the same chemotype, and the adverse effect was reversed.
Ten cats received cannabis as a single therapy. Diseases included gingivostomatitis, dermatopathies, oncologic disease, pain, asthma, and signs and symptoms produced by two pathologies. Data are shown in Fig. 6B. Doses of cannabinoids were received for polymedicated patients, and those that received only oil were not significantly different (Supplemental Table 3). Like in the dog’s group, veterinarians and caregivers perceived a reduction of clinical signs and symptoms at 15, 30, and 60 days of treatment (Fig. 7B).
Then, we analyzed whether the type of food influenced the improvement in clinical conditions in both groups. Supplemental Table 4 shows, for dogs and cats, the proportion of animals that presented different grades of improvement related to the total of animals fed using raw food, cooked food, ultra-processed, and mixed diets. In dogs and cats (Table S4), more than 50% of animals showed significant improvement independently of the type of diet. To evaluate whether the type of food was related to the improvement during the treatment, we compared the number of animals that showed mild/moderate or significant improvement according to the food consumed, looking for possible drug-food interaction. The relationship between these variables was not significant, Χ2 (3, N = 89) = 3.2527, p = 0.3542 for dogs, and Χ2 (3, N = 24) = 2.7563, p = 0.4307 for cats. According to these data, feeding is not associated with the response during the treatment.